Could not find what you are looking for?
- Treatments & Procedures
- Cholecystectomy (Gall Bladder Removal) Surgery - Procedure, Cost, Indications, Risks, and Benefits
Cholecystectomy (Gall Bladder Removal) Surgery - Procedure, Cost, Indications, Risks, and Benefits

Cholecystectomy (Gall Bladder Removal) Surgery - Everything you need to know
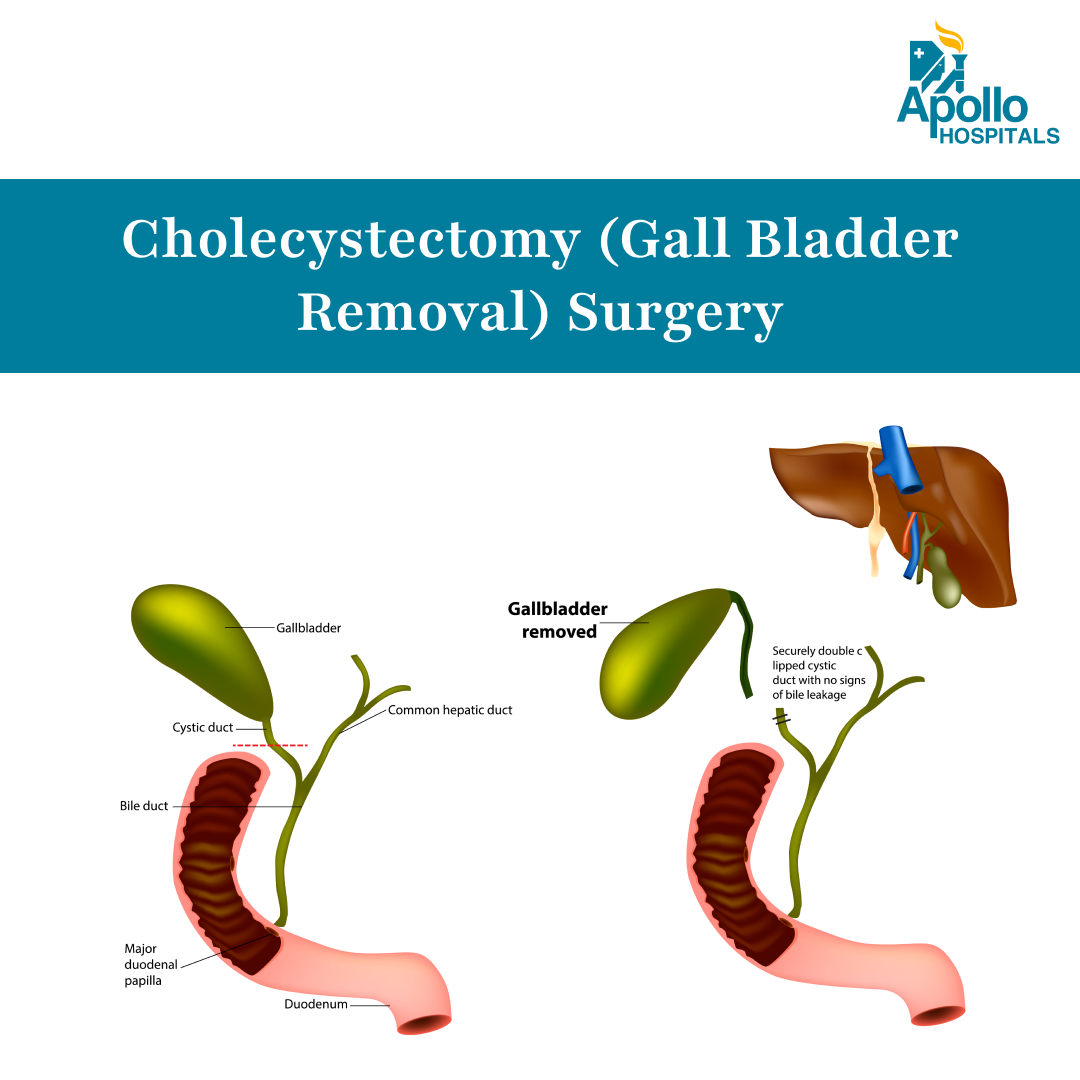
What is Cholecystectomy (Gall Bladder Removal)?
Cholecystectomy is a surgical procedure that involves the removal of the gallbladder, which is a small organ located beneath the liver. The gallbladder is responsible for storing bile, a digestive fluid produced by the liver. This surgery can be performed either through a large open incision in the abdomen (open cholecystectomy) or through small keyhole incisions using a camera and instruments (laparoscopic cholecystectomy). Both approaches aim to treat gallbladder-related conditions, and the choice of method depends on several factors, including the patient's overall health, anatomy, and presence of complications.
The primary purpose of Cholecystectomy is to alleviate symptoms associated with gallbladder disease and to prevent potential complications. Gallstones can lead to severe pain, infections, and even pancreatitis if they block the bile ducts. By removing the gallbladder, the source of these issues is eliminated, allowing for improved digestive health and overall well-being.
Cholecystectomy is usually recommended when other less invasive treatments, such as medication or dietary changes, have failed to provide relief. It is a well-established procedure that has been performed for decades, and while minimally invasive techniques like laparoscopic cholecystectomy are often preferred due to faster recovery, open Cholecystectomy remains a vital option for certain patients, especially those with complex anatomy, prior surgeries, or severe inflammation.
Why is Cholecystectomy Done?
Cholecystectomy is typically indicated for patients experiencing significant symptoms related to gallbladder disease. The most common condition leading to this procedure is cholecystitis, which is the inflammation of the gallbladder, often caused by gallstones. Patients may present with symptoms such as:
- Severe abdominal pain, particularly in the upper right quadrant
- Nausea and vomiting
- Fever and chills
- Jaundice (yellowing of the skin and eyes)
- Indigestion or bloating after meals
In some cases, gallstones can migrate into the bile ducts, leading to a condition known as choledocholithiasis—a situation where stones obstruct the bile ducts, potentially causing serious complications such as bile duct infections or pancreatitis. When these symptoms are severe or recurrent, and when imaging studies (like ultrasound or CT scans) confirm the presence of gallstones or inflammation, a Cholecystectomy may be recommended.
The decision to proceed with Cholecystectomy is often made after careful consideration of the patient's overall health, the severity of symptoms, and the potential risks and benefits of the surgery. In emergency situations, such as acute cholecystitis, the procedure may be performed urgently to prevent further complications.
Types of Cholecystectomy
Cholecystectomy refers to the surgical removal of the gallbladder. The type of procedure chosen depends on factors such as the patient’s medical history, anatomy, severity of gallbladder disease, and the surgeon’s recommendation. The main types include:
Laparoscopic Cholecystectomy (Minimally Invasive)
This is the most commonly performed approach today. It involves small incisions in the abdomen, through which a camera and surgical instruments are inserted to remove the gallbladder.
Benefits include:
- Shorter hospital stay (often same-day discharge or 24-hour admission)
- Faster recovery (typically 1 to 2 weeks)
- Less post-operative pain
- Lower risk of complications compared to open surgery
It is usually recommended for patients with uncomplicated gallbladder issues, such as gallstones or mild inflammation.
Single-Incision Laparoscopic Cholecystectomy (SILC)
This is a variation of the laparoscopic method, where the entire procedure is performed through a single incision, usually at the navel.
Potential advantages:
- Better cosmetic results
- Reduced post-operative discomfort
However, SILC is not suitable for all patients, particularly those with obesity or complicated gallbladder disease. It requires advanced surgical expertise and is available at select centers, including Apollo Hospitals.
Robotic-Assisted Cholecystectomy
This technique uses robotic technology to assist in gallbladder removal. The surgeon operates from a console, controlling robotic arms with high precision.
Advantages include:
- Enhanced 3D visualization and dexterity
- Greater precision in complex or high-risk cases
- Minimal tissue trauma
It is often used in patients with challenging anatomy, obesity, or when conventional laparoscopy poses increased risks. This option is available in select Apollo Hospitals equipped with robotic surgical platforms.
Which Procedure Is Right for You?
The decision depends on multiple factors:
- Type and severity of gallbladder disease
- Past abdominal surgeries
- Patient’s overall health, BMI, and comorbidities
- Availability of technology and surgical expertise
At Apollo Hospitals, our experienced team ensures a patient-centric approach, tailoring the surgical plan to maximize safety, comfort, and recovery outcomes.
Indications for Cholecystectomy
Several clinical situations and diagnostic findings can indicate the need for Cholecystectomy. These include:
- Cholecystitis: Acute or chronic inflammation of the gallbladder is the most common indication for this surgery. Patients may experience severe pain, fever, and tenderness in the abdomen.
- Gallstones: The presence of gallstones that cause recurrent pain or complications, such as pancreatitis or cholangitis, can necessitate the removal of the gallbladder.
- Biliary Obstruction: If gallstones block the bile ducts, leading to jaundice or infection, Cholecystectomy may be required to relieve the obstruction.
- Pancreatitis: In cases where gallstones are the cause of pancreatitis, removing the gallbladder can help prevent future episodes.
- Gallbladder Polyps: Large or symptomatic gallbladder polyps may warrant removal to rule out cancer or other serious conditions.
- Previous Abdominal Surgery: Patients with a history of extensive abdominal surgery may not be suitable candidates for laparoscopic techniques, making open Cholecystectomy a more viable option.
- Obesity or Other Health Conditions: Patients with obesity or other comorbidities may have a higher risk of complications with laparoscopic surgery, leading some surgeons to consider open Cholecystectomy, although obesity alone is not a direct indication for surgery.
- Inability to Visualize the Gallbladder: In some cases, the gallbladder may not be easily visualized during laparoscopic surgery due to anatomical variations or inflammation, necessitating conversion to an open procedure.
In summary, Cholecystectomy is indicated for patients with significant gallbladder-related symptoms, complications from gallstones, or specific anatomical considerations that make laparoscopic surgery challenging. The decision to proceed with this surgery is made collaboratively between the patient and their healthcare team, ensuring that all factors are considered for optimal outcomes.
Contraindications for Cholecystectomy
Cholecystectomy is a surgical procedure to remove the gallbladder, typically performed when a patient has gallstones or gallbladder disease. However, certain conditions may make a patient unsuitable for this surgery. Understanding these contraindications is crucial for both patients and healthcare providers.
- Severe Cardiac or Pulmonary Conditions: Patients with significant heart disease, such as severe coronary artery disease or heart failure, may not tolerate the stress of surgery. Similarly, those with chronic obstructive pulmonary disease (COPD) or other serious lung conditions may face increased risks during and after the procedure.
- Obesity: While obesity itself is not an absolute contraindication, morbid obesity can complicate the surgery. Excess body weight can increase the risk of complications, such as infection and delayed healing, and may make the surgical procedure technically more challenging.
- Coagulation Disorders: Patients with bleeding disorders or those on anticoagulant therapy may be at higher risk for excessive bleeding during and after surgery. These patients require careful evaluation and management before considering Cholecystectomy.
- Severe Infections: If a patient has an active infection, particularly in the abdominal area, it may be unsafe to proceed with surgery. Infections can complicate the healing process and increase the risk of postoperative complications.
- Advanced Liver Disease: Patients with severe liver dysfunction or cirrhosis may not be suitable candidates for Cholecystectomy due to the increased risk of complications, including bleeding and poor wound healing.
- Pregnancy: While surgery during pregnancy is not ideal, it is not considered an absolute contraindication. Laparoscopic cholecystectomy can be safely performed during the second trimester if the benefits outweigh the risks. The timing and necessity of surgery during pregnancy should be evaluated carefully by the medical team.
- Previous Abdominal Surgeries: Patients with extensive scar tissue from previous surgeries may face increased risks of complications, such as injury to surrounding organs or difficulty accessing the gallbladder.
- Patient Refusal: If a patient is not fully informed about the procedure and its risks or refuses to consent to surgery, it cannot be performed.
Understanding these contraindications helps ensure that Cholecystectomy is performed safely and effectively, minimizing risks for patients.
How to Prepare for Cholecystectomy
Preparation for Cholecystectomy is essential to ensure a smooth surgical experience and optimal recovery. Here are the key steps and considerations for patients:
- Pre-Operative Consultation: Before the surgery, patients will meet with their surgeon to discuss the procedure, risks, and benefits. This is an excellent time to ask questions and clarify any concerns.
- Medical History Review: Patients should provide a complete medical history, including any medications, allergies, and previous surgeries. This information helps the healthcare team assess risks and tailor the surgical approach.
- Physical Examination: A thorough physical examination will be conducted to evaluate the patient’s overall health and identify any potential issues that could affect the surgery.
- Laboratory Tests: Blood tests, including a complete blood count (CBC) and liver function tests, are typically performed to assess the patient’s health and ensure they are fit for surgery. Additional tests, such as imaging studies, may also be ordered.
- Medication Management: Patients may need to adjust their medications before surgery. For example, blood thinners may need to be temporarily stopped to reduce the risk of bleeding. It’s crucial to follow the surgeon’s instructions regarding medication management.
- Dietary Restrictions: Patients are usually advised to follow a specific diet leading up to the surgery. This may include avoiding solid foods for a certain period and adhering to a clear liquid diet the day before the procedure.
- Fasting: Most surgeons will require patients to fast for at least 8 hours before the surgery. This means no food or drink, including water, to reduce the risk of aspiration during anesthesia.
- Arranging Transportation: Since Cholecystectomy is performed under general anesthesia, patients will need someone to drive them home after the procedure. It’s important to arrange for a responsible adult to assist.
- Post-Operative Care Planning: Patients should prepare for their recovery by arranging for help at home, especially during the first few days after surgery. This may include assistance with daily activities and meal preparation.
- Understanding Recovery: Patients should be informed about what to expect after surgery, including pain management, activity restrictions, and follow-up appointments. Knowing what to expect can help ease anxiety and promote a smoother recovery.
By following these preparation steps, patients can help ensure that their Cholecystectomy is successful and that they are well-equipped for recovery.
Cholecystectomy: Step-by-Step Procedure
Cholecystectomy is a well-established surgical procedure that involves several key steps. Here’s a straightforward overview of what happens before, during, and after the surgery:
- Before the Procedure:
- Arrival at the Hospital: Patients will arrive at the hospital on the day of the surgery. They will check in and may be asked to change into a hospital gown.
- Pre-Operative Assessment: A nurse will take vital signs and may insert an intravenous (IV) line to administer fluids and medications.
- Anesthesia Consultation: An anesthesiologist will meet with the patient to discuss anesthesia options and address any concerns.
- Final Preparations: Patients will be asked to sign consent forms, confirming their understanding of the procedure and its risks.
- During the Procedure:
- Anesthesia Administration: Once in the operating room, the patient will receive general anesthesia, ensuring they are completely unconscious and pain-free during the surgery.
- Incision: The surgeon will make a large incision in the right upper abdomen, typically about 6 to 8 inches long, to access the gallbladder.
- Gallbladder Removal: The surgeon will carefully detach the gallbladder from the liver and surrounding structures, removing it from the body. If gallstones are present in the bile duct, they may also be addressed at this time.
- Closure: After the gallbladder is removed, the surgeon will inspect the area for any bleeding and then close the incision with sutures or staples. A sterile dressing will be applied.
- After the Procedure:
- Recovery Room: Patients will be taken to a recovery room, where they will be monitored as they wake up from anesthesia. Vital signs will be checked regularly.
- Pain Management: Pain relief will be provided as needed, and patients may receive medications through the IV or orally.
- Hospital Stay: Most patients stay in the hospital for 1 to 3 days, depending on their recovery progress and any complications.
- Discharge Instructions: Before going home, patients will receive instructions on wound care, activity restrictions, and dietary recommendations. It’s important to follow these guidelines to promote healing.
- Follow-Up Care: Patients will have a follow-up appointment with their surgeon to monitor recovery and address any concerns. This is an important step in ensuring a successful outcome.
By understanding the step-by-step process of Cholecystectomy, patients can feel more prepared and informed about their surgical experience.
Risks and Complications of Cholecystectomy
Like any surgical procedure, Cholecystectomy carries certain risks and potential complications. While many patients undergo the surgery without issues, it’s important to be aware of both common and rare risks.
Common Risks:
- Infection: There is a risk of infection at the incision site or within the abdominal cavity. Signs of infection may include fever, increased pain, or redness around the incision.
- Bleeding: Some bleeding is expected, but excessive bleeding may require additional treatment or a blood transfusion.
- Pain: Postoperative pain is common and can usually be managed with medications. However, some patients may experience prolonged discomfort.
- Nausea and Vomiting: These symptoms can occur after anesthesia and may be managed with medications.
Rare Risks:
- Bile Duct Injury: Accidental injury to the bile duct can occur during surgery, leading to complications such as bile leaks or strictures. This may require further surgical intervention.
- Gallbladder Remnants: In some cases, small pieces of gallbladder tissue may be left behind, potentially leading to continued symptoms or the need for additional surgery.
- Blood Clots: Patients are at risk for developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) after surgery, especially if they are immobile for extended periods.
- Anesthesia Complications: Although rare, complications related to anesthesia can occur, including allergic reactions or respiratory issues.
Long-Term Risks:
- Digestive Changes: Some patients may experience changes in digestion after gallbladder removal, such as diarrhea or difficulty digesting fatty foods. These symptoms often improve over time.
- Chronic Pain: A small number of patients may develop chronic abdominal pain after surgery, which can be challenging to manage.
While the risks associated with Cholecystectomy are important to consider, it’s essential to remember that the benefits of the procedure often outweigh these risks for patients with significant gallbladder issues. Cholecystectomy can provide relief from pain and prevent complications associated with gallstones, leading to improved quality of life. Always discuss any concerns with your healthcare provider to make an informed decision about your treatment options.
Recovery After Cholecystectomy
Recovering from an Cholecystectomy is a crucial phase that requires attention and care. The expected recovery timeline typically spans several weeks, with most patients experiencing significant improvement within the first two weeks post-surgery. Initially, patients may stay in the hospital for 2 to 5 days, depending on their overall health and any complications that may arise.
During the first week, it’s common to experience pain and discomfort around the incision site. Pain management is essential, and your healthcare provider will prescribe medications to help alleviate this discomfort. It’s important to follow the prescribed pain management plan and communicate any concerns with your doctor.
After the first week, many patients can gradually resume light activities, such as walking and basic household tasks. However, it’s crucial to avoid heavy lifting, strenuous exercise, or any activity that puts pressure on the abdomen for at least 4 to 6 weeks. Full recovery can take up to 6 to 8 weeks, during which time you should monitor your incision for signs of infection, such as increased redness, swelling, or discharge.
Aftercare tips include:
- Follow-Up Appointments: Attend all scheduled follow-up appointments to ensure proper healing.
- Wound Care: Keep the incision clean and dry. Follow your surgeon's instructions on how to care for the wound.
- Dietary Adjustments: Start with a bland diet and gradually reintroduce regular foods as tolerated. Avoid fatty and spicy foods initially.
- Hydration: Drink plenty of fluids to stay hydrated, especially if you experience any digestive changes.
- Rest: Prioritize rest and avoid overexertion to facilitate healing.
Most patients can return to normal activities, including work, within 4 to 6 weeks, but this can vary based on individual recovery rates and the nature of their job. Always consult your healthcare provider before resuming any strenuous activities.
Benefits of Cholecystectomy
Cholecystectomy offers several key health improvements and quality-of-life outcomes for patients suffering from gallbladder-related issues. One of the primary benefits is the effective removal of gallstones and the gallbladder itself, which can alleviate symptoms such as severe abdominal pain, nausea, and digestive disturbances.
Patients often report significant relief from symptoms post-surgery, leading to an improved quality of life. The procedure can also prevent potential complications associated with gallstones, such as pancreatitis or cholecystitis, which can be serious and require more extensive treatment.
Another benefit is the ability to address other abdominal issues during the same surgery. If a patient has other conditions, such as hernias or adhesions, the surgeon can often treat these simultaneously, reducing the need for additional surgeries in the future.
Moreover, Cholecystectomy is a well-established procedure with a high success rate. While it involves a larger incision compared to laparoscopic methods, it allows surgeons to have a better view and access to the abdominal cavity, which can be particularly beneficial in complex cases.
Overall, the benefits of Cholecystectomy include:
- Effective resolution of gallbladder-related symptoms
- Prevention of serious complications
- Potential for simultaneous treatment of other abdominal conditions
- High success rate and established surgical technique
Cholecystectomy vs. Laparoscopic Cholecystectomy
While Cholecystectomy is a traditional method for gallbladder removal, laparoscopic cholecystectomy is a minimally invasive alternative that many patients consider. Below is a comparison of the two procedures:
|
Feature |
Cholecystectomy |
Laparoscopic Cholecystectomy |
|
Incision Size |
Larger incision (6–8 inches) |
Small incisions (0.5–1 inch) |
|
Recovery Time |
6–8 weeks |
1–2 weeks |
|
Hospital Stay |
2–5 days |
1–2 days |
|
Pain Level |
Generally higher post-operative pain |
Lower post-operative pain |
|
Risk of Complications |
Slightly higher due to larger incision |
Lower risk due to minimally invasive approach |
|
Visibility for Surgeon |
Better visibility for complex cases |
Limited, but adequate for most cases |
|
Cost |
Generally higher due to longer hospital stay |
|
Both procedures have their pros and cons, and the choice between them often depends on the patient's specific condition, overall health, and the surgeon's recommendation.
What is the Cost of a Cholecystectomy in India?
The cost of Cholecystectomy in India typically ranges from ₹1,00,000 to ₹2,50,000. Costs may vary depending on the hospital, location, room type, and associated complications.
To know the exact cost, contact us now.
Cholecystectomy in Apollo Hospitals India offers significant cost savings compared to Western countries, with immediate appointments and better recovery times.
Explore affordable Cholecystectomy options in India with this essential guide for patients and caregivers
Frequently Asked Questions
1. What should I eat after a Cholecystectomy?
After a Cholecystectomy, begin with a bland diet (rice, toast, bananas) and gradually reintroduce regular foods. Avoid fatty, fried, or spicy foods for a few weeks to help your digestive system adjust.
2. How long will I stay in the hospital after a Cholecystectomy?
Hospital stay after a Cholecystectomy in India typically lasts 1 to 3 days for laparoscopic surgery and up to 5 days for open procedures, depending on recovery and any complications.
3. When can I return to work after a Cholecystectomy?
Most patients return to work within 1 to 2 weeks after laparoscopic Cholecystectomy. If your job involves physical labor, you may need up to 4–6 weeks to fully recover.
4. Are there dietary restrictions before undergoing Cholecystectomy?
Yes. Prior to Cholecystectomy, your doctor may recommend fasting or a clear liquid diet. Always follow the preoperative instructions provided at Apollo Hospitals or your chosen facility.
5. What pain management is provided after Cholecystectomy?
Post-Cholecystectomy pain is usually managed with prescribed medications. Over-the-counter painkillers may be used, but consult your doctor before taking any.
6. Can I drive after Cholecystectomy surgery?
Avoid driving for at least 1–2 weeks after a Cholecystectomy, especially if you're on pain medication that may impair alertness.
7. What signs of infection should I watch for after a Cholecystectomy?
Watch for redness, swelling, discharge at the incision site, fever, or increasing pain. Report any of these to your Apollo Hospitals care team or local provider promptly.
8. Is it safe to exercise after a Cholecystectomy?
Light walking is encouraged soon after surgery. Avoid strenuous activity or lifting heavy objects for at least 4–6 weeks, especially after an open Cholecystectomy.
9. How does digestion change after Cholecystectomy?
You may experience temporary bloating or diarrhea after gallbladder removal. These symptoms usually improve within a few weeks as your body adapts.
10. Can I take my regular medications after Cholecystectomy?
Most medications can be resumed after surgery. However, consult your surgeon, especially if you’re on blood thinners, diabetes medication, or antihypertensives.
11. Is nausea normal after Cholecystectomy surgery?
Yes. Mild nausea is common and typically temporary. If persistent, consult your Apollo Hospitals team or doctor for anti-nausea options.
12. Will I need to make long-term dietary changes after Cholecystectomy?
Most people return to a normal diet. However, a low-fat, high-fiber diet with small, frequent meals may help optimize digestion after gallbladder removal.
13. Is Cholecystectomy riskier for obese patients?
Obesity may increase the risk of complications during and after Cholecystectomy. At Apollo Hospitals, advanced laparoscopic techniques help reduce these risks significantly.
14. Can diabetics undergo Cholecystectomy safely?
Yes, but diabetics require careful blood sugar management before and after Cholecystectomy to reduce infection and healing risks. A multidisciplinary team at Apollo ensures safety.
15. What precautions should hypertensive patients take before Cholecystectomy?
Blood pressure should be well controlled before undergoing Cholecystectomy. Your doctor may adjust medications temporarily around the surgery period.
16. Is fatigue normal after Cholecystectomy?
Yes. Feeling tired for a few days to weeks post-surgery is common. Adequate rest and a gradual return to activity help with recovery.
17. Can I shower after my Cholecystectomy?
Yes, you can usually shower within 24–48 hours. Avoid soaking the incision or swimming until the wound is fully healed.
18. Can I care for children after Cholecystectomy?
You may need assistance with childcare, especially lifting or active care, during the first 2–3 weeks of recovery.
19. How do I manage constipation after Cholecystectomy?
Drink plenty of fluids, consume fiber-rich foods, and consider a stool softener if needed. Pain medication can slow bowel movements, so adjustments may help.
20. Do I need follow-up visits after a Cholecystectomy?
Yes. Follow-up appointments are important to ensure proper healing and discuss any issues like pain, digestion changes, or medication adjustments.
21. How does Cholecystectomy in India compare to surgery abroad?
Cholecystectomy in India, especially at hospitals like Apollo, offers high-quality care with advanced laparoscopic techniques at a more affordable cost compared to many Western countries.
22. Is laparoscopic Cholecystectomy available in India?
Yes, laparoscopic Cholecystectomy is widely performed in India and is the preferred method due to its faster recovery and fewer complications. Apollo Hospitals specializes in this approach.
23. Are Indian surgeons trained for advanced Cholecystectomy procedures?
Yes. Surgeons at leading hospitals like Apollo are internationally trained and experienced in both laparoscopic and complex Cholecystectomy cases.
24. Can I travel after Cholecystectomy?
Avoid long-distance travel for at least 2–4 weeks after surgery. Get your doctor’s clearance before flying, especially if you're recovering from an open Cholecystectomy.
25. What if I have a history of gallstones before my Cholecystectomy?
A history of gallstones is often the reason for surgery. Post-surgery, symptoms usually resolve completely. Inform your doctor if symptoms persist.
26. . I’ve had a C-section. Can I still undergo a Cholecystectomy?
Yes, many women undergo Cholecystectomy after a Cesarean delivery without complications. However, the surgeon will consider any scar tissue or adhesions from the previous surgery, especially if it was open (non-laparoscopic). At Apollo Hospitals, our experienced laparoscopic surgeons are trained to navigate such complexities safely.
27. I’ve had a hysterectomy. Will that affect my Cholecystectomy?
A previous hysterectomy, especially abdominal, may lead to internal scar tissue or changes in pelvic anatomy. However, it doesn’t typically prevent Cholecystectomy. The surgical team will review imaging and surgical history to avoid complications.
28. I’ve had hernia surgery before. Will that complicate gallbladder removal?
If you've had an umbilical or incisional hernia repair, especially with mesh, it may require extra care during laparoscopic entry.
29. I’ve undergone bariatric (weight-loss) surgery. Can I still have a Cholecystectomy?
Yes, but the approach may vary based on the type of bariatric surgery (e.g., gastric bypass, sleeve gastrectomy). Some patients develop gallstones after rapid weight loss, making Cholecystectomy necessary.
30. What replaces the gallbladder after it is removed in a Cholecystectomy?
Nothing physically replaces the gallbladder after a Cholecystectomy. The liver continues to produce bile, but instead of being stored in the gallbladder, the bile flows directly into the small intestine. Most people adapt well to this change, though some may notice temporary digestive changes as the body adjusts.
31. Is it safe to undergo Cholecystectomy during pregnancy?
Cholecystectomy during pregnancy is generally safe when medically necessary, especially in the second trimester. If gallbladder issues like gallstones cause severe pain, infection, or complications, doctors may recommend surgery to protect both the mother and baby. The team at Apollo Hospitals carefully evaluates each case to ensure the safest outcome for pregnant patients.
Conclusion
Cholecystectomy is a significant surgical procedure that can greatly improve the quality of life for individuals suffering from gallbladder issues. Understanding the recovery process, benefits, and potential alternatives can empower patients to make informed decisions about their health. If you or a loved one is considering this procedure, it’s essential to consult with a medical professional to discuss your specific situation and ensure the best possible outcomes.